Scientists have created cyborg embryos by implanting electrode arrays into the developing brains of frogs, mice, and salamanders. Although the researchers reject implants in human embryos as unethical, they suggest their technology might one day help study and treat neurodevelopmental conditions in children. The stretchable technology at the core of the electrode arrays could record brain activity while remaining soft enough to accommodate the children’s growth.
Recording the activity of neurons during brain development can help scientists “understand how the brain transforms from a piece of tissue into a computing machine,” says Jia Liu, an assistant professor of bioengineering at Harvard University. “Virtually all neural technology was developed for the adult brain, but there are so many questions left unanswered about the developing brain.”
However, until now, there has been no way for researchers to record neural activity throughout the entire brain on the cellular level on millisecond time scales throughout development. For instance, functional magnetic resonance imaging (fMRI) can scan the entire brain, but it has low resolution in space and time. Previous research using electrode arrays implanted in the brain yielded high resolution in space and time across the brain, but the way in which embryonic brains can rapidly change meant that such devices could not stay accurate over time.
Flexible Brain Probes for Embryos
In 2015, Liu and his colleagues developed flexible, minimally invasive brain probes. This led Liu to wonder if these pliant electronics might keep up with the mutable nature of embryonic brains. However, our brains and those of other vertebrates are complex, three-dimensional structures, and so embedding any electrodes into their interiors would inflict at least some damage during implantation.
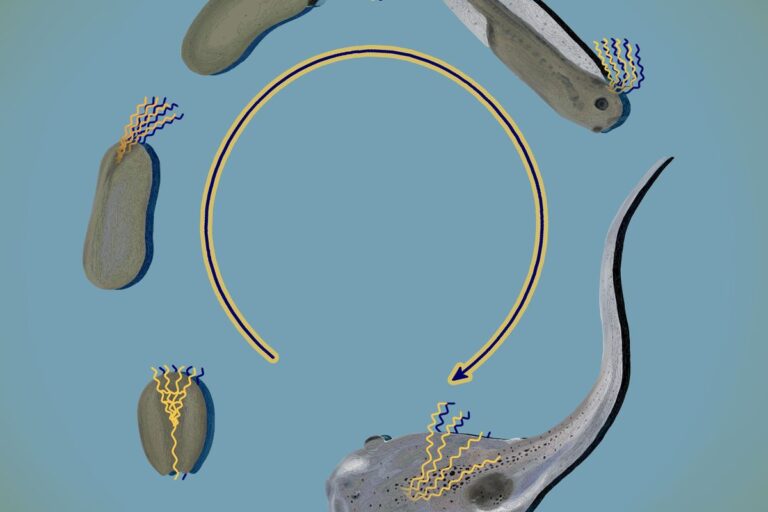
In the new study, Liu and his colleagues overcame this problem by implanting electrodes into developing brains when these were still two-dimensional layers of stem cells. Over the course of development, these sheets of cells fold into 3D structures, and the electronic meshes fold with them, distributing electrodes throughout the brain and creating what the scientists dub cyborg embryos. Their research was published online today in Nature.
In the team’s first experiments, the electrode arrays were flexible, but they were still too rigid to prove compatible with embryonic development “and easily cut the embryonic tissue,” Liu says. He and his colleagues had to rely on even softer materials called fluorinated elastomers, which could stretch and keep pace with the dynamic tissues. The resulting flexible mesh electronics are less than one micrometer thick.
In experiments with frog and salamander embryos, the new arrays can record neuron electrical activity on millisecond scales across the brain throughout development in a stable, continuous manner. Exams of neural tissues and the activity of stress-related genes found these electrodes had no discernible impact on brain development or function, nor did behavioral tests, such as whether tadpoles with the arrays avoided incoming objects. In preliminary tests, the scientists also implanted their devices into mouse embryos and newborn rats and recorded neural activity in developing mammalian brains.
Analysis of the frog embryos showed how neural activity varied over development. The early brain displayed slow, global synchronized activity, but over time, different brain regions showed distinct and faster dynamics, and ultimately cell-specific behavior. “Studying how neural dynamics change during development could prove useful for developing better machine learning algorithms,” Liu says.
The salamanders the researchers examined, known as axolotls, possess the ability to regenerate virtually any part of their body, including neural systems. In experiments where the scientists cut the tails of axolotl tadpoles, they found that during regeneration, neural activity in the brain significantly increased, becoming similar to what was seen during the early stages of embryonic development. “This suggests that brain activity might play a role in regeneration,” Liu says. “It would be very interesting to see if we can control the central nervous system to facilitate this kind of tissue recovery or injury recovery.”
Liu stresses that “we are not talking about implants in human embryos, which is completely unethical and not our intention at all.” However, he suggests their electronics could still find use in children to help study or even treat neurodevelopmental conditions “in applications where you need the technology to be stretched and extremely soft to accommodate brain development.”