Around ten years ago, fantastic media coverage of 3D printing dramatically increased expectations for the technology. A particular darling of that coverage was the use of 3D-printing for prosthetic limbs: For example, in 2015, The New York Times celebrated the US $15 to $20 3D-printed prosthetic hands facilitated by the nonprofit E-nable, which paired hobbyist 3D printer owners with children with limb differences. The magic felt undeniable: disabled children could get cheap, freely accessible mechanical hands made by a neighbor with an unusual hobby. Similar stories about prosthetics abounded, painting a picture of an emerging high-tech utopia enabled by a technology straight out of Star Trek.
But as so often happens, the Gartner Hype Cycle was in full force. By the mid-2010s, 3D-printing was in the “Peak of Inflated Expectations” phase, and prosthetics was no exception. Those LEGO-style hands getting media attention didn’t have the strength needed for a wearable device, the prints themselves had too many inaccuracies, and the designs were—as you may imagine an entirely plastic object to be—deeply uncomfortable.
 Quorum’s 3D-printed prostheses socket.Quorum
Quorum’s 3D-printed prostheses socket.Quorum
The so-called “Trough of Disillusionment” followed. Joe Johnson, CEO of Quorum Prosthetics in Windsor, Colorado, saw prosthetists shy away from 3D printing technologies for years. Johnson stuck it out, though, waiting for technology and bureaucracy to catch up to his ambition. A milestone happened last year when U.S. medical insurers released an “L-code” last year specifically for adjustable sockets for prosthetic limbs. An L-code allows durable medical equipment—such as prosthetics—to be handled for billing within the U.S. insurance system. Quorum’s engineers responded with a sophisticated, adjustable socket utilizing 3D printing. Quorum’s design can adjust both volume and compression on residual limbs, making a better fit, like tightening your shoe laces.
Despite its high-tech and sleek appearance, Johnson says his socket could be made using traditional methods. But 3D printing makes it a “bit better and easier.” “When you look at overall cost of labor,” says Johnson, “it just keeps going up. To manufacture one of our sockets would take a technician 12 or 16 hours to make [using traditional methods].” Using 3D printing, he says “we can make five overnight.” As a result, Quorum spends less on technician labor.
However, there are new costs. Quorum needs to pay for software subscriptions and licenses on top of the overhead required to operate a nearly one-million dollar Hewlett-Packard 3D printer. “We have to spend $50,000 on the A/C unit just to control the humidity,” says Johnson. At the end of the day, it costs over $1000 to print each socket, even when they print multiple sockets together. The costs are actually now higher than if Quorum didn’t use 3D printing to manufacture prostheses, but Johnson believes the quality is superior. “You can see more patients. [3D printing] is so precise and less adjustments need to be made.” This has meant fewer follow-up visits for patients and, for many, better fits.
 Operation Namaste is using 3D printing to standardized the liners for prosthetic limb sockets.Operation Namaste
Operation Namaste is using 3D printing to standardized the liners for prosthetic limb sockets.Operation Namaste
Why hasn’t 3D printing lowered costs?
When I asked Jeff Erenstone, a prosthetist for over two decades and founder of prosthetic limb non-profit Operation Namaste, why 3D printed designs hadn’t lowered costs, he said Quorum is “able to make a socket that was not possible before 3D printing—very next level socket and sophistication. What they are making isn’t lowering costs any more than Ferrari is lowering costs. They are making the Ferrari of sockets.”
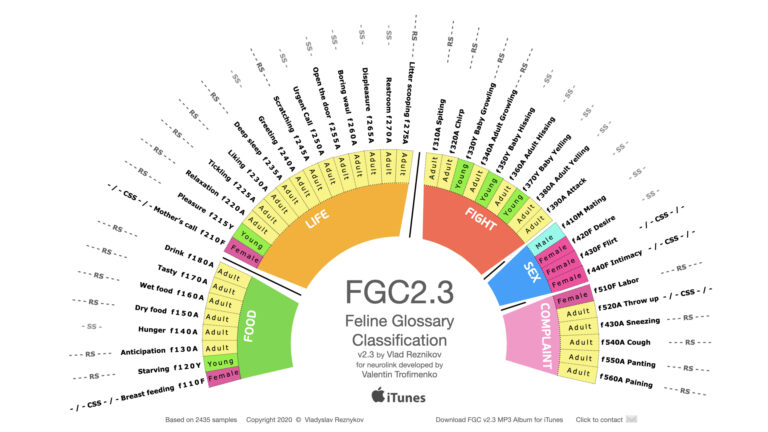
But Erenstone says the technology is finally getting closer to achieving some of the things everyone imagined was possible ten years ago. Namely, the ability to share designs around the world and increase communication between practitioners has been life-changing. Ernestone set his sights on cracking the code around prosthetic liners—the silicone, flexible socks that prosthesis-users roll up onto their residual limb before inserting it into the prosthesis socket. Liners from one of the most common brands, Ossur, are sold for many hundreds of dollars each, but are vital for a prosthetic to be comfortable enough to wear all day. To bring high quality liners to prosthesis-users in low-resourced countries, Operation Namaste is standardizing the molds to make silicone liners. Clinicians anywhere in the world can print the mold using inexpensive 3D printers and about $22 in materials and local labor costs to produce a high-quality silicone liner. “3D printing has value in low income countries because accessibility is so much harder,” explains Erenstone. “I have not seen it [have as much value] in the urban areas where there is adequate prosthetic care.”
3D printing has been especially helpful in war zones such as Ukraine and Sudan, where it may be unsafe for prosthetists to visit from abroad and there are very few resources. Canada-based Victoria Hand Project identifies prosthetics and orthotics clinics around the world, sets them up with a 3D print lab, and trains the clinicians in 3D printing software. Where 3D printing has made a difference is increasing knowledge sharing between practitioners and increasing the availability of low-cost designs. It is unclear, however, whether prosthetics printed with cheaper 3D printers hold up compared to conventional time-tested, body-powered, low-cost designs. Quorum Prosthetics operates a nonprofit called One Leg at a Time in Tanzania, where they train local people in 3D scanning and measuring of residual limbs, but these scans are sent back to Colorado, where an industrial multi-jet fusion printer actually prints the hands. Local Tanzanians may be trained to use the new technology, but the best equipment to finish the task is still out of their reach.
 Unlimited Tomorrow’s TrueLimbUnlimited Tomorrow
Unlimited Tomorrow’s TrueLimbUnlimited Tomorrow
Can 3D-printed prosthetics be cheaper?
The goal of using 3D printing to make prosthesis less expensive is still being pursued, but non-technical issues pose significant obstacles. Easton LaChapelle, founder of Unlimited Tomorrow, sought to leverage 3D printing—a technology he fell in love with as a teenager—to create a high-functioning, low-cost hand to rival the clunky multi-articulating prosthetic hands on the market. The result was the TrueLimb, a $7,000 prosthetic hand so intricate in its appearance it looks as if it was carved from wood. The TrueLimb was sold directly to consumers in an effort to bypass the headaches of medical insurance, but even at $7,000—about 1/10th the cost of other multi-articulating myoelectric hands—the hand proved too expensive for many. Customers approached LaChapelle and asked for them to take insurance. Unlimited Tomorrow then started working with prosthetists who had to decide between billing insurance companies for (for example) a German-made prosthetic hand for tens of thousands of dollars versus the TrueLimb. “Prosthetists were hesitant to work with us because our price point was so low, they couldn’t mark it up to what they are used to,” explains LaChapelle. “It doesn’t matter what the technology is in these circumstances. Unlimited Tomorrow could have produced the best device, but clinicians are like ‘why would I bill for a TrueLimb when I could bill a Bebionic?’” As a result, TrueLimb’s cost shot up.
Soon enough, says LaChapelle, “We became exactly the problem we tried to solve. We were just another fancy arm that cost a bunch of money and for the consumer there was still an out of pocket expense.” LaChapelle decided it was unethical to continue this way and has put Unlimited Tomorrow “on pause.” In the meantime, he’s working on commercializing some of the innovations he and his team of engineers stumbled upon along the way, such as their haptic glove system, which they hope will take hold in virtual reality applications. “The US [prosthetics] market is not gonna change,” he says with dismay. With the profits from their glove, he hopes to focus on developing a “badass body-powered [prosthetic] device” to distribute through a nonprofit.
The insurance companies are innovating, too, and not in a helpful way. While 3D printed devices now have official, codified L-codes that prosthetists across the US can bill, Joe Johnson says insurance companies don’t care about the benefits of 3D printed devices. “The lawyers have reached a level of sophistication of writing policy that they can write around mandates [that should guarantee coverage],” Johnson explains. “We have certain prosthetic mandates for coverage but the insurance companies have become very sophisticated. They’re betting on you giving up.” Insurance companies still refuse to cover even microprocessor-enabled knees, says Johnson, a technology which is going on twenty-five years old. He and his team entertained the possibility of trying to recycle microprocessor knees to increase their affordability to many patients. In a not-to-distant future, they imagined insurance companies would find new ways to thwart their efforts. Says Johnson: “They’d totally brick those knees.”
This article was supported by the IEEE Foundation and a John C. Taenzer fellowship grant.










 Quorum’s 3D-printed prostheses socket.Quorum
Quorum’s 3D-printed prostheses socket.Quorum Operation Namaste is using 3D printing to standardized the liners for prosthetic limb sockets.Operation Namaste
Operation Namaste is using 3D printing to standardized the liners for prosthetic limb sockets.Operation Namaste Unlimited Tomorrow’s TrueLimbUnlimited Tomorrow
Unlimited Tomorrow’s TrueLimbUnlimited Tomorrow